Introduction
Are you experiencing tooth pain or sensitivity? It might be a cavity. Understanding what a cavity looks like can help you identify the problem early and seek treatment before it worsens.
Cavities, also known as dental caries, are decayed areas on the teeth that result from the breakdown of tooth enamel. They usually appear as small, dark spots on the surface of the tooth. However, not all cavities are visually apparent, especially in the early stages. Some may be hidden between the teeth or in hard-to-reach areas, making them difficult to identify without a dental examination.
If left untreated, cavities can progress and cause deeper damage to the tooth, leading to severe pain, infection, or tooth loss. This is why early detection and preventive measures are crucial. Routine dental check-ups and practicing good oral hygiene can help prevent cavities and detect them in their earliest stages.
Causes of Cavities

Cavities are primarily caused by poor oral hygiene and an unhealthy diet. When we consume sugary or starchy foods and beverages, the bacteria in our mouths feed on the sugars and produce acids. These acids, combined with the bacteria and food particles, form plaque, a sticky film that adheres to the teeth.
Over time, the acids in plaque can demineralize the tooth enamel, resulting in the formation of cavities. Poor oral hygiene habits, such as inadequate brushing and flossing, allow plaque to accumulate and increase the risk of cavities. Additionally, factors like dry mouth, genetic predisposition, and certain medications can also contribute to cavity formation.
Signs and Symptoms of Cavities
Recognizing the signs and symptoms of cavities is essential for early detection and treatment. While some cavities may be painless, others can cause discomfort and sensitivity. Here are some common symptoms to watch out for:
Tooth sensitivity: You may experience sensitivity to hot or cold foods and beverages, as well as sweet or acidic substances. This sensitivity occurs when the protective enamel layer is damaged, exposing the underlying dentin and nerve endings.
Toothache: Cavities can cause persistent or intermittent toothaches that may worsen when biting down or consuming sugary foods. The pain can vary in intensity and may indicate that the cavity has reached the inner layers of the tooth.
Visible holes or pits: In more advanced stages, cavities can cause visible holes or pits on the surface of the affected tooth. These may appear as dark spots or stains and can be seen with the naked eye.
It’s important to note that not all cavities present with visible signs, especially in the early stages. Regular dental check-ups and X-rays are crucial for detecting hidden cavities and preventing further damage.
The Stages of Cavity Development

Cavity development occurs in several stages, starting from the initial demineralization of the tooth enamel to the formation of a full-blown cavity. Understanding these stages can help you identify cavities early on and take appropriate action.
Demineralization: This is the initial stage where the tooth enamel begins to lose minerals due to acid exposure. At this stage, the enamel may appear intact, but it is weakened and more susceptible to decay.
Enamel decay: As demineralization progresses, the enamel breaks down, forming small white spots on the tooth surface. These spots indicate the presence of early-stage cavities and should be addressed promptly to prevent further damage.
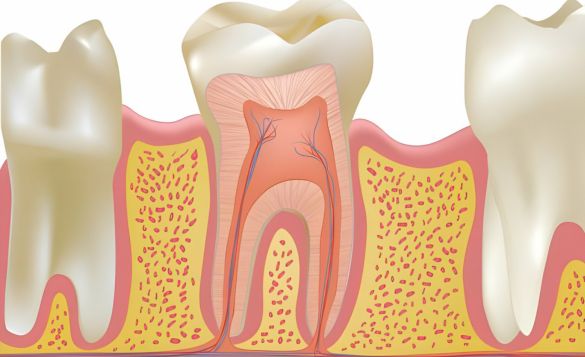
Dentin decay: If left untreated, cavities can progress deeper into the tooth, reaching the dentin layer. Dentin is softer than enamel and decays at a faster rate. The cavity may cause increased tooth sensitivity and mild to moderate pain at this stage.
Pulp involvement: When the cavity reaches the pulp, which contains nerves and blood vessels, it can cause severe pain, infection, and abscess formation. At this stage, root canal treatment or tooth extraction may be necessary to alleviate the symptoms and prevent further complications.
How to Prevent Cavities
Prevention is always better than cure when it comes to cavities. By incorporating these preventive measures into your daily routine, you can significantly reduce the risk of cavities:
Brushing and flossing: Brush your teeth at least twice a day using fluoride toothpaste and a soft-bristled toothbrush. Floss daily to remove plaque and food particles from between your teeth and along the gumline.
Limit sugary and acidic foods: Minimize your consumption of sugary and acidic foods and beverages, such as candies, sodas, and citrus fruits. If you do indulge, rinse your mouth with water afterward or brush your teeth to remove any residual sugars or acids.
Use fluoride products: Fluoride helps strengthen tooth enamel and make it more resistant to decay. Use fluoride toothpaste, or mouthwash, or ask your dentist about professional fluoride treatments.
Drink plenty of water: Water helps wash away food particles and neutralize acid levels in the mouth. Drink fluoridated tap water whenever possible, as it can also provide additional protection against cavities.
Maintain a balanced diet: Include a variety of nutritious foods in your diet, such as fruits, vegetables, dairy products, and lean proteins. A well-balanced diet provides essential nutrients for healthy teeth and gums.
Dental Care for Cavity Prevention
In addition to practicing good oral hygiene and following a healthy diet, regular dental care plays a crucial role in cavity prevention. Here are some dental care recommendations to keep your teeth in optimal condition:
Schedule regular dental check-ups: Visit your dentist every six months for routine dental check-ups and professional cleanings. These visits allow your dentist to detect cavities early on and provide necessary treatments.
Dental sealants: Dental sealants are thin protective coatings applied to the chewing surfaces of the back teeth (molars and premolars). They create a barrier that prevents plaque and food particles from settling in the grooves and pits, reducing the risk of cavities.
Fluoride treatments: Your dentist may suggest fluoride treatments to strengthen your tooth enamel and provide extra protection against cavities. These treatments involve applying a fluoride varnish, gel, or foam to the teeth.
X-rays: Dental X-rays are useful for detecting cavities that may not be visible during a visual examination. Your dentist will recommend the appropriate frequency of X-rays based on your oral health needs.
Treatment Options for Cavities

The treatment for cavities depends on the extent and severity of decay. In the early stages, cavities can often be treated with less invasive procedures, while advanced cavities may require more extensive treatments. Here are the common treatment options for cavities:
Dental fillings: Dental fillings are the most common treatment for small to moderate-sized cavities. The decayed portion of the tooth is removed, and the resulting cavity is filled with a dental material such as composite resin, amalgam, or porcelain.
Dental crowns: When a cavity is too large to be restored with a filling, a dental crown may be recommended. A crown is a custom-made cap that covers the entire tooth, providing strength and protection.
Root canal therapy: If the cavity has reached the pulp, root canal therapy may be necessary to save the tooth. The infected pulp is removed, and the root canals are cleaned, filled, and sealed. A crown is often placed on the treated tooth to restore its appearance and function.
Tooth extraction: In cases where the cavity has caused extensive damage or the tooth is beyond repair, extraction may be the only option. After the extraction, your dentist may recommend tooth replacement options like dental implants, bridges, or dentures.
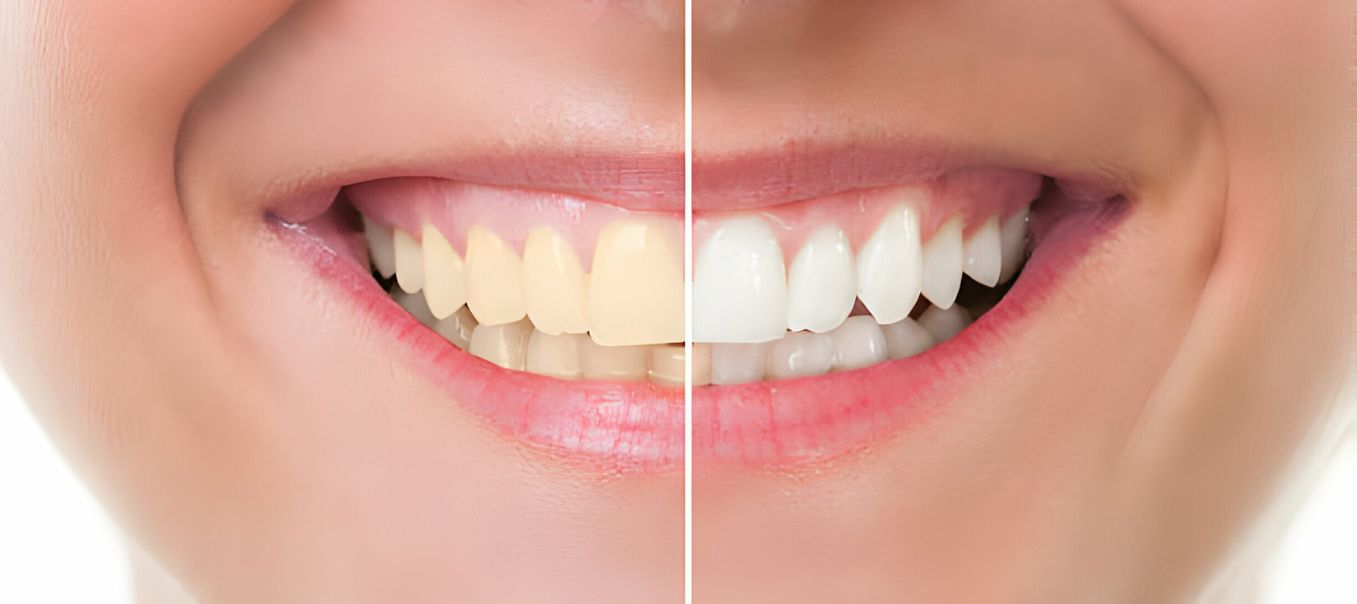
What Do Cavities Look Like?
Cavities can vary in appearance depending on their size, location, and stage of development. In the early stages, they may appear as small white spots or stains on the tooth surface. As the decay progresses, the cavities can become darker and more noticeable, appearing as brown, black, or grey spots. In some cases, cavities can cause visible holes or pits on the tooth surface.
However, it’s important to note that not all cavities are visually apparent, especially in the early stages. Some may be hidden between the teeth or in hard-to-reach areas, making them difficult to identify without a dental examination. Regular dental check-ups and X-rays are essential for detecting hidden cavities and preventing further damage.
Conclusion
Understanding what a cavity looks like is crucial for early detection and timely treatment. Cavities can appear as small dark spots, stains, or visible holes on the tooth surface. However, not all cavities are visually apparent, making regular dental check-ups and preventive measures essential.
By practicing good oral hygiene, maintaining a healthy diet, and seeking regular dental care, you can significantly reduce the risk of cavities and maintain optimal oral health. Remember, prevention is key when it comes to cavities, so take proactive steps to protect your teeth and smile brightly for years to come.
Frequently Asked Questions
A cavity appears as a dark spot or shadow on an X-ray, indicating areas of tooth decay where the enamel has been compromised.
Cavities on molars may appear as dark or discolored spots on the surface of the tooth, often accompanied by sensitivity or pain.
In the early stages, a cavity may manifest as a white spot on the tooth surface, indicating demineralization and the onset of decay.
After a cavity is filled, the restoration may appear as a tooth-colored filling or amalgam material, blending seamlessly with the natural tooth structure.
A cavity on an X-ray typically appears as a dark area within the tooth, indicating decay or erosion of the tooth structure.
A filled cavity may appear as a smooth, uniform surface on the tooth, restoring its shape and function while blending with the surrounding enamel.
Cavities on molars may present as dark spots or pits on the chewing surface, often accompanied by discomfort or sensitivity to hot or cold stimuli









Leave a Reply